DWELL BEYOND THE ORDINARY
Intramedullary nail techniques play a crucial role in fracture healing. As per recent reports, over 2 million fractures occur annually in the United States alone. The use of Nail Intramedullari devices has transformed the approach to these injuries. Studies indicate a 90% success rate in proper alignment and stability when using intramedullary nails, making them a preferred choice.
However, there are challenges that orthopedic surgeons face. Complications such as infection and nonunion still occur, affecting 5-10% of cases. Surgeons must navigate these risks while ensuring optimal healing. Detailed analysis of nail designs can reveal advantages. Some nails provide angular stability, while others focus on flexibility.
The selection of the right intramedullary nail and technique directly impacts patient outcomes. Failures often prompt reevaluation of surgical methods. Continuous education and skill enhancement are vital for surgeons to maximize the benefits of Nail Intramedullari methods.
Intramedullary nailing is a widely used technique for treating fractures, especially in long bones. Studies show that it allows for faster healing and better alignment. According to a 2021 report by the Journal of Orthopedic Trauma, 87% of patients show significant improvement within six months post-surgery. This technique minimizes damage to surrounding soft tissues and preserves blood supply, which can be crucial for healing.
However, challenges remain. Surgeons must carefully choose nail lengths and diameters to fit each patient's unique anatomy. Improper sizing can lead to complications. Additionally, there's always the risk of non-union or malunion, which affects about 5% of cases, according to a clinical review in the BMC Musculoskeletal Disorders. Continuous refinement of techniques is essential, as some surgeons express concerns over difficulty in accurately placing the nails.
The choice of fixation method also plays a role. Some studies recommend considering biomechanical properties when selecting nails. Recent data suggests that more rigid fixation can promote quicker healing. However, excessive rigidity may lead to stress shielding. This prompts ongoing research into balancing stability and flexibility for optimal fracture healing. Understanding these nuances can significantly influence surgical outcomes and long-term care strategies.
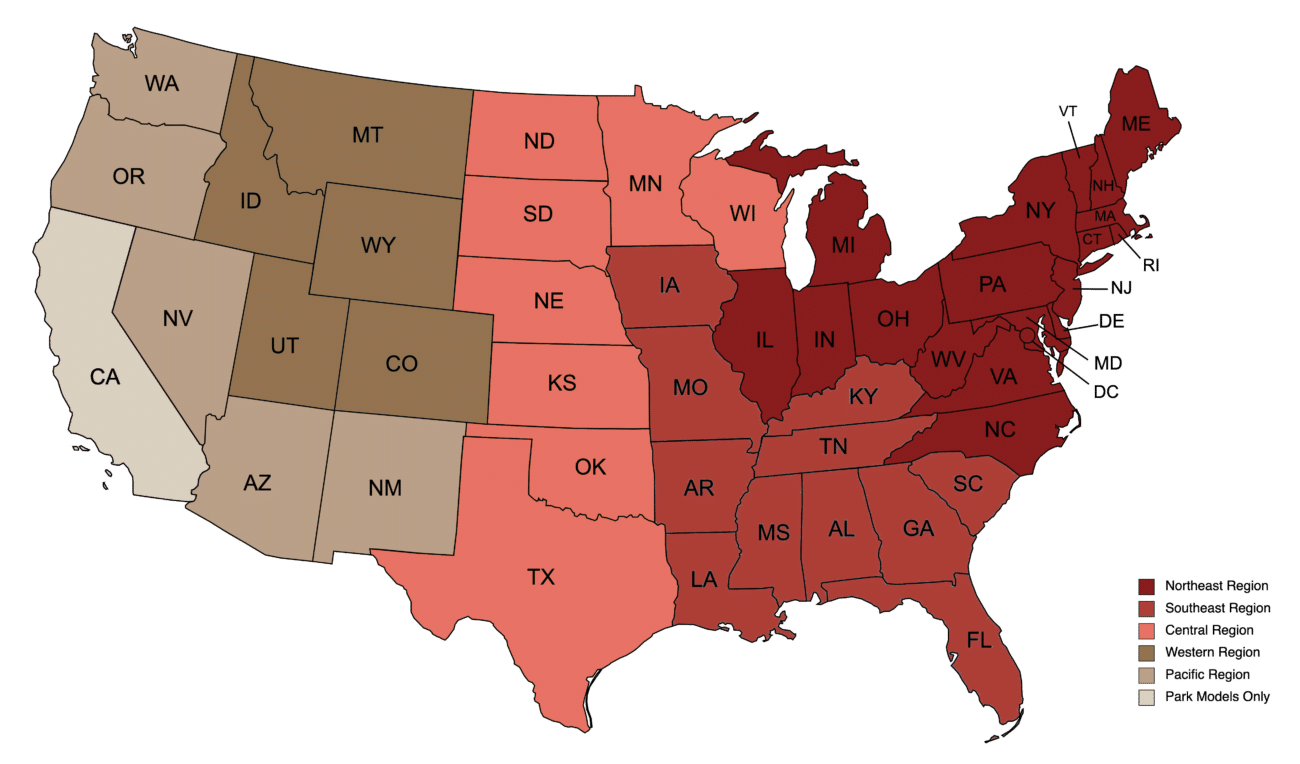
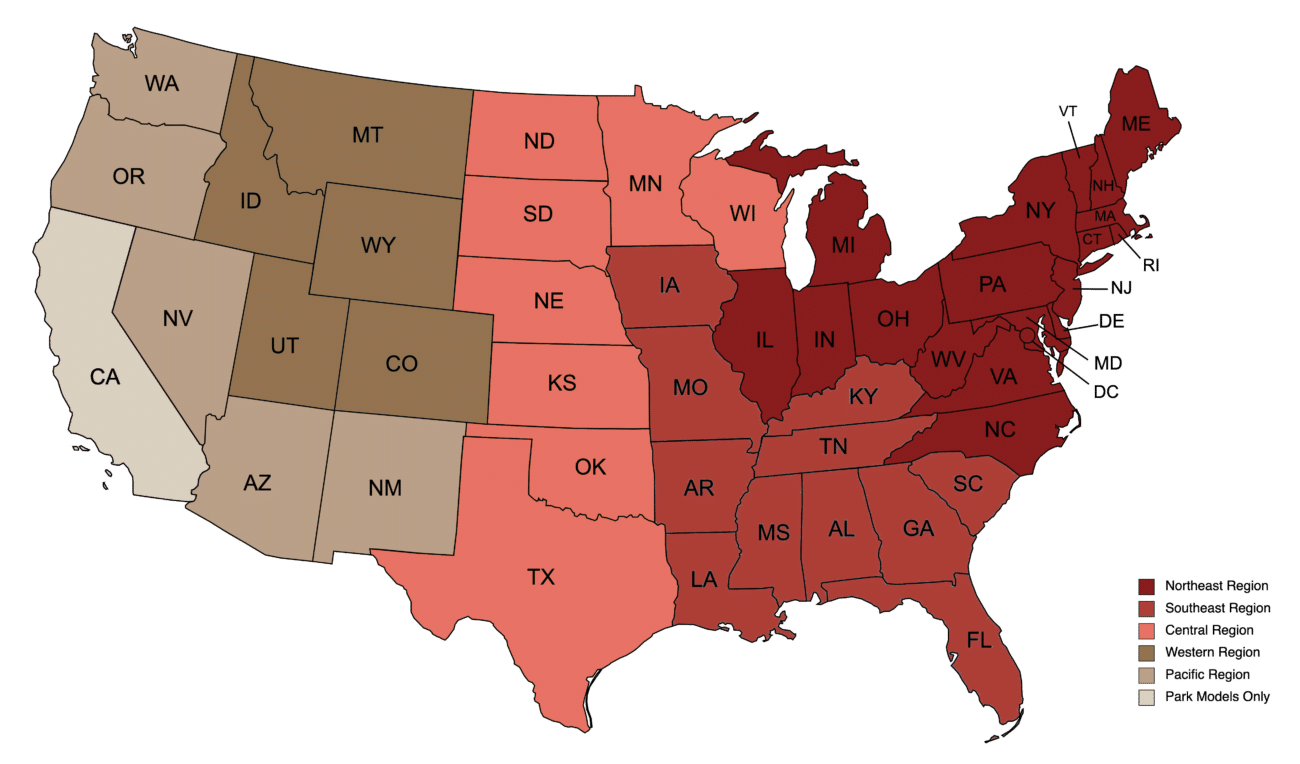
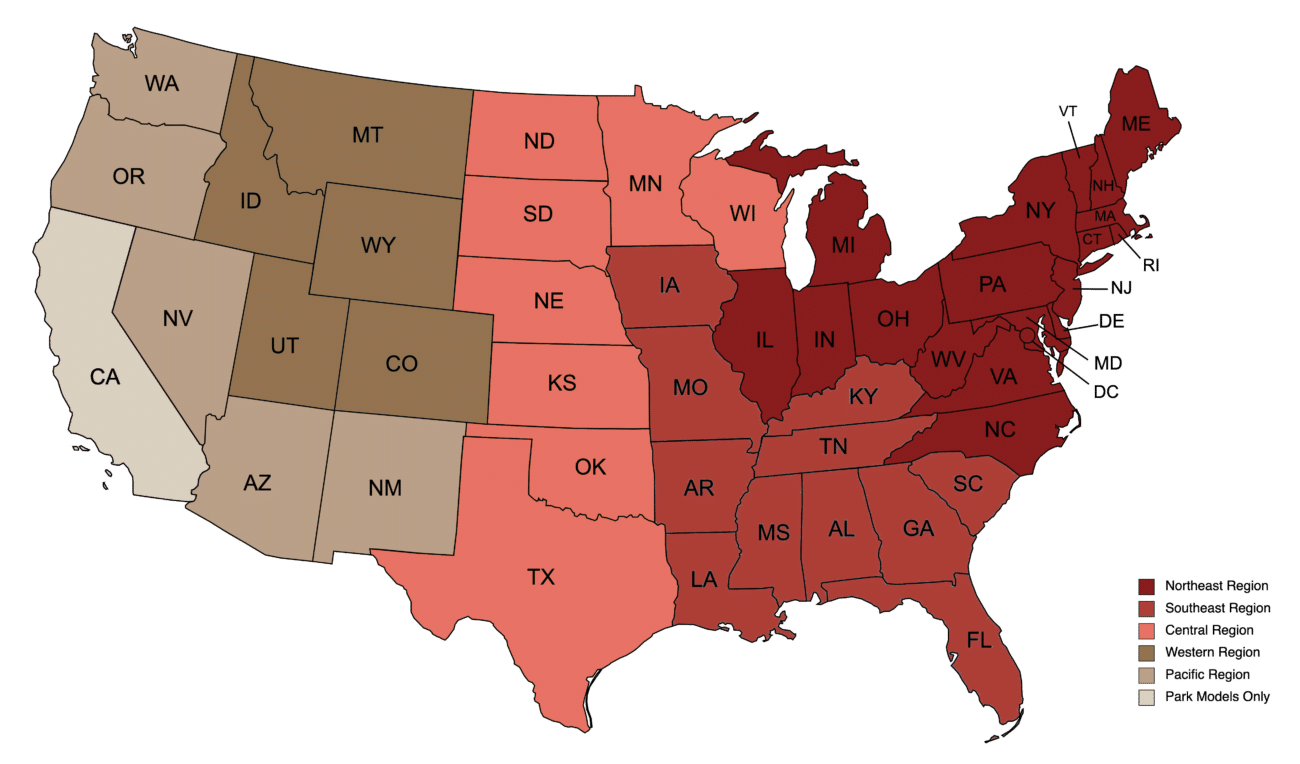
This chart illustrates the effectiveness of various intramedullary nail techniques on fracture healing based on clinical outcomes.
Intramedullary nails have become essential tools in fracture treatment. They are particularly effective for certain types of fractures. These include femoral and tibial fractures. The alignment of these bones is crucial for healing. Intramedullary nails help maintain this alignment. Their ability to support internal fixation is a major benefit. However, not every fracture should use this method.
Indications include unstable fractures or those needing surgical intervention. Patients with multiple fractures often benefit from this technique. Complications can arise, though. Infection is a notable risk. Also, misalignment during insertion can lead to issues. Surgeons must carefully assess each case. Proper imaging and evaluation are key. They ensure that intramedullary nails are indeed the right choice.
The advantages are clear, yet challenges remain. Each patient's situation is unique. Decisions should balance the benefits against potential risks. It’s important to reflect on the individual needs of the patient. Understanding the limitations of intramedullary nails is essential for optimal outcomes.
Intramedullary nailing has become a standard technique for treating long bone fractures. Surgeons need to master key surgical techniques for successful insertion. Proper alignment is crucial. Attention to the patient's anatomy helps achieve this. An accurate entry point allows for better nail placement.
A step often overlooked is adequate reaming. It ensures the nail fits snugly within the medullary canal. However, too much reaming can lead to complications. It's important to find a balance between stability and bone preservation. Surgeons should also consider the size of the nail. Using the wrong size can compromise the healing process.
Surgeons must be mindful of post-operative care too. Monitoring for signs of infection is vital. Early detection can prevent serious issues later on. Additionally, the rehabilitation protocol should be tailored to the individual. Each patient is different, and a one-size-fits-all approach may not yield the best results. Continuous reflection on techniques and outcomes can lead to improvements in practice.
Postoperative care is crucial for successful recovery after intramedullary nail surgery. Patients often feel anxious about the healing process. Regular follow-up appointments help monitor progress. Doctors will check for any complications and adjust care as needed. It’s essential to pay attention to pain levels and swelling. These signs can indicate healing or potential issues.
Tips for postoperative care include maintaining proper hygiene around the surgical site. Keep the area clean and dry to prevent infection. Avoid soaking the wound in water until cleared by a doctor. Ice packs can help reduce swelling. However, don't apply ice directly to the skin.
Rehabilitation is a key part of healing. Engage in gentle exercises as advised by the healthcare provider. These exercises improve mobility and strengthen muscles. It’s important not to rush the rehabilitation process. Listen to your body and rest when needed. Keep a diary of your recovery journey. Reflect on how your body feels each day. This helps track progress and identify any concerns. Focusing on gradual improvements can boost morale during recovery.
| Technique | Indication | Expected Healing Time | Postoperative Care | Rehabilitation Strategies |
|---|---|---|---|---|
| Antegrade Intramedullary Nailing | Femoral shaft fractures | 6-12 weeks | Pain management, wound care | Early mobilization, physical therapy |
| Retrograde Intramedullary Nailing | Distal femoral and tibial fractures | 8-14 weeks | Regular follow-ups, managing complications | Weight-bearing exercises, manual therapy |
| Locked Intramedullary Nailing | Complex or unstable fractures | 8-16 weeks | Monitoring for infection, rehabilitation exercises | Strengthening and range of motion activities |
| Unreamed Intramedullary Nailing | Certain types of fractures in patients with infection | 4-10 weeks | Preventing muscle atrophy, pain management | Gradual reintroduction of activity, physiotherapy |
Intramedullary nailing is a common technique for treating fractures. It offers several advantages, including less soft tissue damage and quicker rehabilitation. However, outcomes can vary significantly based on technique and surgeon experience. A recent study indicated that complication rates can range from 5% to 30% depending on the fracture type and nail insertion angle.
One notable risk involves malalignment. A misalignment of even a few degrees can affect long-term function. A study published in a leading orthopedic journal showed that 12% of patients experienced malunion following intramedullary nailing. This suggests an urgent need for improved training and technique refinement. Surgeons must consider various factors, like the patient's anatomy and fracture pattern, to minimize these risks.
Furthermore, complications like infection and hardware failure remain critical issues. Data shows that approximately 3% of patients develop deep infection issues after the procedure. Addressing these concerns requires a multidisciplinary approach, including pre-operative planning and post-operative care. Continuous assessment of techniques and outcomes is essential to improve patient safety and enhance the effectiveness of intramedullary nailing.
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach, and not, when I came to die, discover that I had not lived.”
- Henry David Thoreau
